Mask mandates are being lifted across the U.S. as COVID infections continue to drop.
“But we’re not in the green zone yet,” said Dr. Biswajit Kar, professor of cardiology with McGovern Medical School at UTHealth Houston and Memorial Hermann Hospital-TMC.
He worries that vaccine hesitancy and COVID fatigue might keep people from comprehending the severity of the current situation. The pandemic is still very much in effect, he added.
“The good news is now we can treat COVID more effectively,” Kar said. “And we have vaccines that prevent COVID effectively as well.”
Preventing deaths, lengthy hospitalizations and long-term side effects is where getting vaccinated can make a world of difference. But that’s not all.
“COVID itself affects the heart,” Kar said. “If you are vaccinated, you are protecting against long-term effects on the heart.”
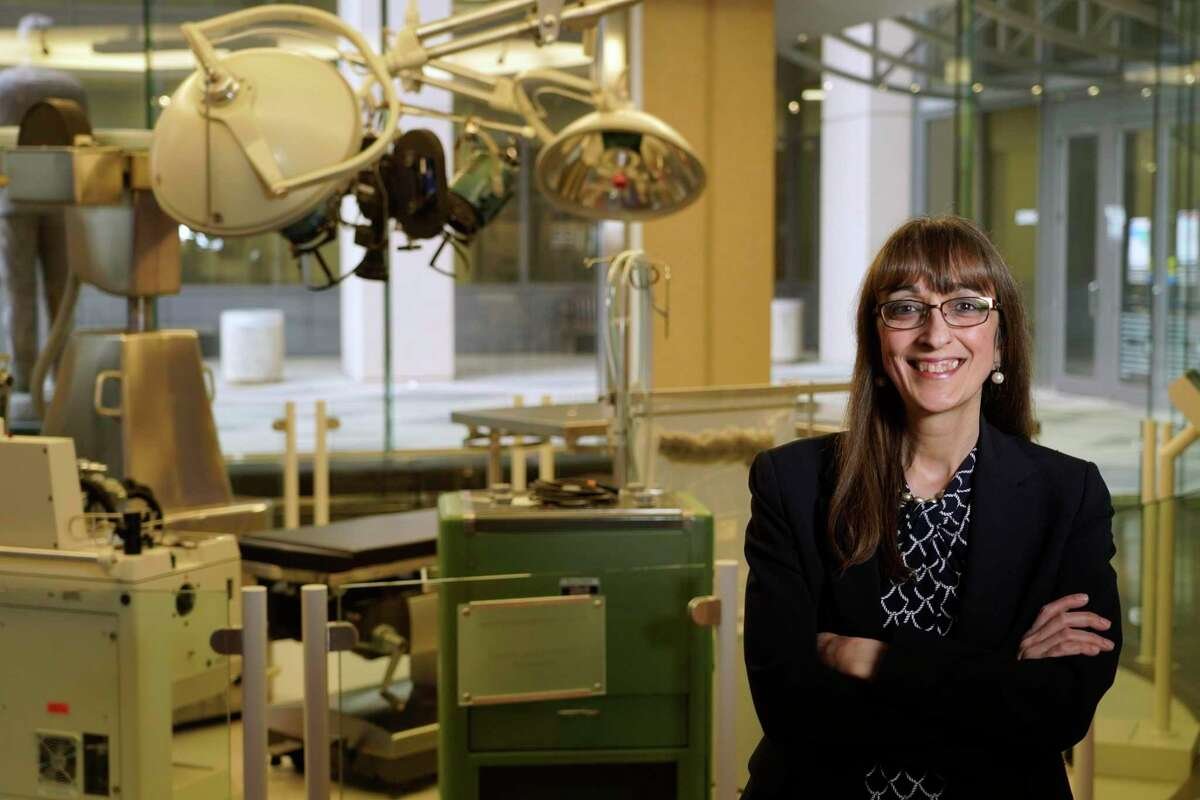
Dr. Biykem Bozkurt, professor of medicine-cardiology at Baylor College of Medicine, said SARS-CoV-2 causes inflammation and injury that can damage a number of organs.
While the lungs might be the first organ that comes to mind while picturing a COVID infection, the heart is also at risk, she said.
“The effects of the infection can be multi-organ related,” Bozkurt said. “It involves not only the lungs but also the brain, the heart and the blood vessels.”
She added that cardiovascular complications of the virus include myocarditis which is inflammation of the heart muscle, pericarditis (swelling and irritation of the thin membrane around the heart), heart attack, arrhythmia, heart failure, cardiac shock and increased danger of blood clot formation in the vascular system throughout the body.
“All of these risk factors are significantly elevated if a person is not vaccinated,” Bozkurt said.
The involvement of the heart in COVID infections has been evident since the beginning of the pandemic, she added.
“The mortality rates are higher with pre-existing conditions like high blood pressure and vascular disease in older individuals, but COVID-19 can also affect the young, healthy and even pediatric populations,” Bozhurt said.
Kar said that COVID can result in both direct and indirect causes for heart complications. The virus can attack the heart, he explained, or can create a cytokine storm, or an overproduction of cytokines, which activate immune cells.
The term “cytokine storm” originated with media reports in the early days of the pandemic, researchers said in JAMA Network, a publication of the American Medical Association. It means there is a hyperactive immune response.
Whenever there’s a cytokine storm, inflammation mediators can affect multiple organs.
“It’s like a nuclear bomb went off in your body,” Kar said.
For instance, heart failure can lead to kidney failure. Or problems with breathing can limit the amount of oxygen in the blood.
“That can suffocate the heart,” Kar said. “Oxygen supply to the heart may be affected by blood clots inside arteries and veins, as well as, severe decrease in oxygenation because of lung damage.”
He said he’s concerned by the myriad complications COVID is causing in the heart — as well as the long-term side effects.
Kar pointed to a German study that looked at patients six months after recovering from a mild case of COVID and found 78 percent had abnormalities on their MRI scans of the heart and 60 percent showed signs of inflammation.
“We do not know what these findings signify, but this is very alarming,” Kar said. “In the worst case scenario, we could be seeing a tsunami of heart attacks in the future. It’s too early to tell.”
Long Covid, or the persistence of symptoms after infection, is still being studied. Physicians continue to report some type of ongoing medical issues with their patients after a COVID diagnosis.
Kar said that long covid is seen more in women. Males, on the other hand, have a higher chance of complications or death from infection of the virus.
COVID ASKED & ANSWERED: Ways you can use the vaccine to fight long COVID-19 symptoms
Bozkurt agreed that long covid can be disabling.
“We’re just getting to understand these risks,” she said. “Recovery can linger in certain individuals. The infection can take a long toll — and results in long-lasting impairment.”
Individuals of all ages can be affected, Bozkurt added, including pediatric populations. Long haul symptoms can develop even in those without pre-existing health conditions.
Kar added that COVID has exposed health inequities. The CDC has documented a higher incidence of infection, hospitalization and death from the virus in Black, Latino, Asian and Native American populations.
“The statistics are staggering,” Kar said.
A racial gap is also evident when it comes to the number of individuals who receive the vaccine or get boosted, Kar added. “There’s a huge disparity,” he said.
Kar hopes there will be greater access to the vaccine — and that demand will stay high.
“Prevention is better than any cure,” he said. “People need to do anything they can to prevent COVID.”
Bozkurt said that the benefits of the vaccine outweigh the risks. Still, some people are worried about side effects.
Rare cases of myocarditis, or inflammation of the heart, have been reported after vaccination. This adverse reaction has been reported predominantly in young, adult males, Bozkurt said.
The cases of myocarditis in those vaccinated, however, are much lower than those seen with COVID infections, Bozkurt said.
And when myocarditis occurs after the vaccine, cases tend to be mild and resolve quickly.
“The vaccines are preventive against infection and also long-term complications of COVID,” Bozkurt said. “The data speaks for itself.”
Managing heart health includes getting vaccinated, the cardiologist said. Getting vaccinations and boosters are key to keeping adverse cardiovascular side effects at bay.
“It is critical to implement all strategies to prevent infection and reduce risk,” she said.
Peyton is a Houston-based freelance writer.